What is Comprehensive Chromosomal Screening (CCS)?
CCS is a screening test to determine if the embryo is more likely ‘normal’ or not prior to embryo transfer. It is done independently of the traditional’ embryo selection ‘methods and Eeva™.
The most common reason that embryos do not implant or later miscarry is that they had a chromosomal abnormality. Rarely, unbalanced embryos will continue to term.
The most common reason an embryo is not normal is egg age (i.e. maternal age) which leads to failed accurate separation of chromosomes during the cell division process (nondisjunction). This leads to an imbalance (too much or too little) of chromosomal DNA material in the embryo.
What is the CCS process?
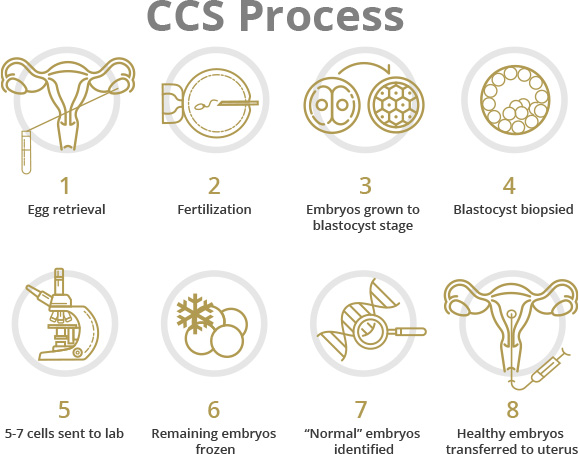
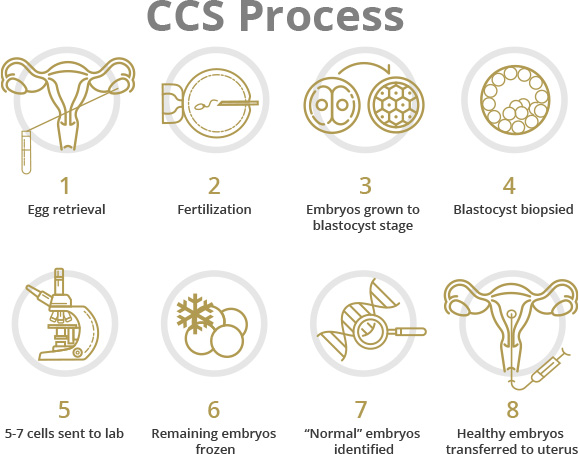
In order to do CCS, the eggs are fertilized and grown to the day 5/6 stage of embryo development (blastocyst). If the embryos do not develop to the blastocyst stage, CCS cannot be done. Some embryos survive to day 5 but do not form blastocysts. Embryos that do not make blastocysts by day 6 are presumed not to be ‘normal’.
At the blastocyst stage, the embryos are biopsied. The biopsy removes 5-7 cells from the trophectoderm (the layer of cells that will become the placenta). The cells that will become the fetus are undisturbed. The embryos are frozen and the biopsy is sent to a genetics lab for analysis.
The analysis determines if the chromosomal complement of the cells that are biopsied is ‘balanced’ or most likely to be ‘normal’ or ‘viable’. CCS testing is reported to have an accuracy of approximately 98%. Literature from genetic testing companies delineate details as information evolves.
CCS does not assess single genes that sit on the chromosomes (e.g. cystic fibrosis or thalassemia). Preimplantation Genetic Diagnosis (PGD testing) is the technique used for determining these single gene diseases.
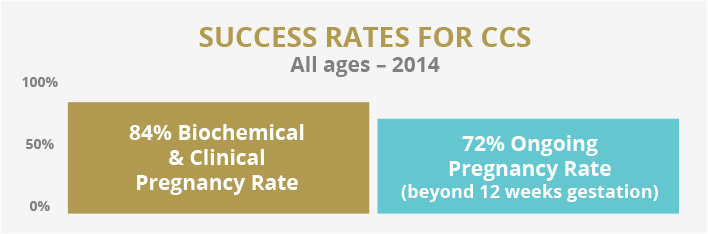
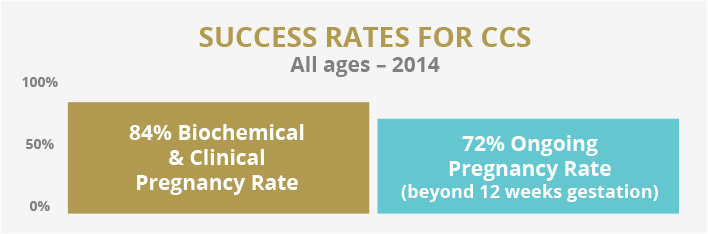
When ‘viable’ embryos are identified, the patient will return for a frozen embryo transfer. When a single ‘viable’ embryo is transferred, the ‘pregnancy rates’ are maximized and miscarriage rates minimized.
Excellent CCS IVF success rates are achieved independently of maternal age if the embryo is known to be ‘normal’ (i.e. a 40 year old woman who transfers a known ‘normal’ embryo will have the same pregnancy rate at a 30 year old woman who transfers a known ‘normal’ embryo).
Indications:
- Recurrent pregnancy loss
- Age > 36 with good ovarian reserve
- Repeated implantation failure
- Multiple failed IVF cycles